Pharma-psychiatry, bipolar disorder, and the IMMDS Review (2 of 3: COI)
(See the previous piece on the IMMDS Review and the RCPsych’s failure to promote it)
In October 2018 Dr David Baldwin FRCPsych, appearing for the Royal College of Psychiatrists (RCPsych), provided written responses to the Review Panel’s written questions. The last of those questions (p. 214) concerned conflict of interest (COI):
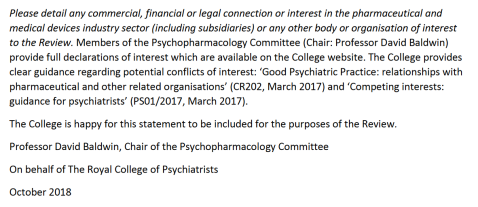
It is false to claim the declarations on the RCPsych website are ‘full’ when they only go back three years. The Review is public, so the meaning of ‘full’ should be as the public would understand it, rather than professionals or academics.
And Dr Baldwin was clearly aware that the IMMDS Review is substantially ‘historical’: in his oral evidence he talked about valproate’s elevated risks being known since the mid-1990s. Therefore his answers about COI should contain information covering decades, not just a few years.
As it happens, Dr Baldwin’s current RCPsych declarations are nearly two years out of date:
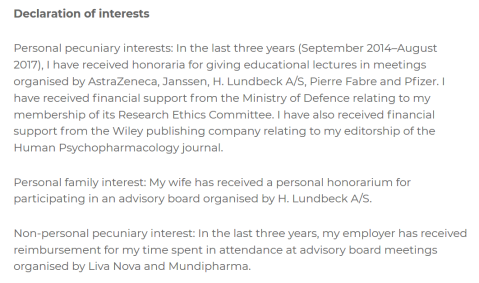
Further, it is absurd to claim that these statements are ‘full’, given that they are unquantified. We actually have Dr Baldwin’s recent quantified declarations on the ABPI’s ‘Disclosure’ site:

I have never seen the RCPsych, any NHS website, or any mental health charity mention the ABPI Disclosure site, so the chances of any patient looking at it before they consult a psychiatrist seem slim. And because disclosure in UK law and GMC guidance and regulation is voluntary, these may only be part-disclosures.
I think the few patients who would look this up in advance would be more wary of psychiatrists who had not disclosed. But because of the law and the GMC’s soft approach, that information is not available.
A patient with FACS, or a relative, researching a psychiatrist who prescribed valproate to a mother, will be unable to find even this incomplete information beyond three years.
Dr Baldwin claimed the RCPsych produces ‘clear guidance’ on COI. It is not ‘clear’. Good Psychiatric Practice states that COI declarations must be made when engaging in ‘college activity’: it does not state whether such declarations should go beyond the usual three years, or whether they should be quantified. In my experience they do not and are not.
For clinical work Good Psychiatric Practice simply refers to the GMC’s Good Medical Practice: to be dealt with in a future piece here.
As for Competing Interests: Guidance for Psychiatrists, I was unable to find such a document on the RCPsych website.
In the oral evidence on 28th January 2019 it is disappointing that the IMMDS Review panel asked Dr Baldwin no questions about COI.
NHS psychiatrist Dr Peter Gordon has been campaigning for compulsory COI declaration laws for years. The RCPsych has refused to comment on the issue, stating that it is ‘a matter for the government’. The GMC failed to respond to his enquiries. In my view these are expressions of contempt towards people experiencing drug and device harms. In late 2018 Dr Gordon resigned his membership of the RCPsych and he later revealed he had been ‘gaslighted’ by the RCPsych, but that his NHS employer supported him.
Dr Gordon has documented Dr Baldwin’s long history of involvement with Pharma, including his promotion of the allegedly ‘defective’ SSRI Seroxat, and its dubious UK licence for ‘Social Anxiety Disorder’, which I recall many ordinary psychiatrists in the 1990s sceptically viewing as a Pharma construct.
It seems likely that my own campaigning on Pharma COI was a factor in my GMC-MPTS suspension, on very dubious grounds. The GMC has still not disclosed the nature of its anonymous psychiatrist investigator’s links to the RCPsych, and it has not interviewed me, seven months after it received the first anonymous complaint about me.
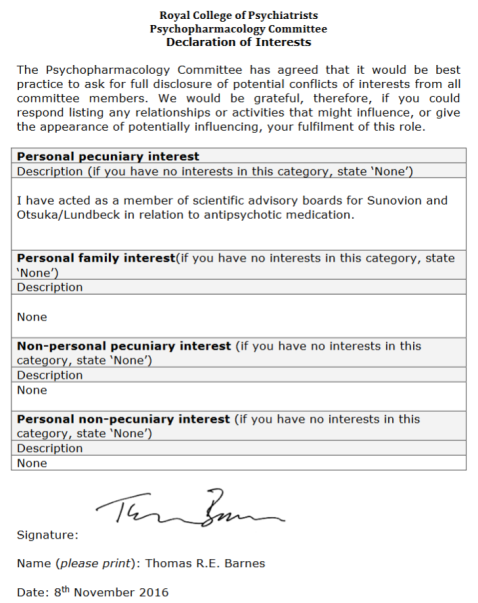
Dr Baldwin mentioned Dr Thomas Barnes FRCPsych, in relation to the POMH survey(s) of prescribing rates of psychiatric drugs in the NHS. Dr Barnes is a member of the psychopharmacology committee and his current COI declaration is even more out of date:
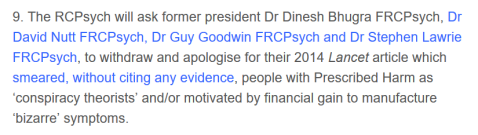
Finally (for this piece on COI), Dr Baldwin mentioned the British Association for Psychopharmacology (BAP) several times, as having views and policies on valproate in line with the RCPsych. The editor of the Journal of Psychopharmacology (BAP’s main journal) is Dr David Nutt FRCPSych. It is interesting to see that Dr Nutt’s latest paper has Dr Baldwin as a co-author. I have criticised Dr Nutt in my ‘Manifesto‘:
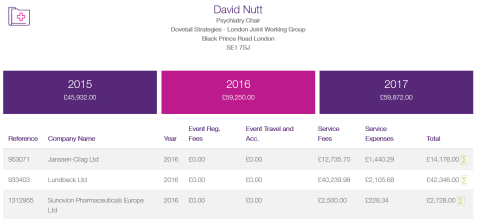
Dr Nutt’s recent ABPI COI voluntary declaration supports the idea that Pharma payments to doctors correlate with a ‘dismissive’ attitude towards patients experiencing drug harms:
Dr Peter Gordon (see above) has published this mildly satirical image of Dr Nutt, based on past drug company interests:

I have defended this use of satire, against the accusation that it is unfairly ‘ad hominem’.
[16th December 2020. I have just noticed that a third piece on bipolar disorder & IMMDSR was not published. That would have been on Dr Baldwin’s failure to submit evidence on the range of opinion on bipolar disorder within the RCPsych, especially the opinion that milder forms of bipolar (‘bipolar 2’) have been promoted under Pharma influence. I will try to find my draft, and publish early next year, as the issue is still relevant.]
Trackbacks / Pingbacks